What is it?
Common Conditions
Symptomatology: Painful stiff shoulder:
If your shoulder is very painful and stiff, it may fall in to one of the following condition:
- Frozen shoulder / Adhesive Capsulitis
- Arthritis of the shoulder joint itself
- Stiffness from previous injury or surgery to the shoulder
Frozen Shoulder / Adhesive Capsulitis: Frozen shoulder can develop spontaneously or from minor injury. There is also a risk of developing this condition following any sort of surgery to the shoulder. Frozen shoulder is a self-resolving condition and will go through three phases as below:>
Phase 1 – the inflammatory phase – this is the worst part of the condition when the shoulder is extremely painful, simple movements or even catching the elbow on a table can be extremely painful. Treatment of this phase is really confined to adequate analgesia and steroid injection for pain relief. This phase can go on for up to six months.
Phase 2 – the frozen phase – as the inflammatory phase resolves the pain should improve to the point where the patient does not require analgesia. At this point the shoulder will still remain quite stiff but there should be a lot less pain. It is at this stage that physiotherapy and possibly surgical intervention may be of benefit.
Phase 3 – the thawing phase – this is where movements will return very slowly and gradually over time. Recovery of all three phases can take anywhere between 12 and 24 months to resolve and generally there is often a loss of 10% global range of movement permanently regardless of whether surgery is performed or not.
Surgery – in order to try and accelerate your recovery, arthroscopic surgery and manipulation of the shoulder may be considered in the frozen phase. This will be carried out as a day case under general anaesthetic and regional anaesthetic to the arm. Three holes are created, the inflammatory tissue is removed and the shoulder gently manipulated. There can be vast improvement in elevation and reaching of the shoulder and on external rotation. Internal rotation (getting the arm around the back to the bra strap for example) is often minimally improved but should improve with time. There is a small risk of fracture with manipulation of any shoulder which is to be expected and the other risks associated with arthroscopy.

Symptomatology: Pain on reaching
This is probably the most common condition seen in my practice and is known as as rotator cuff impingement / tendonopathy. The rotator cuff tendons help to elevate and rotate the shoulder from the waist. Pain on reaching and weakness can involve tears within the tendons. It also includes pain arising from the AC (acromio-clavicular) joint. The pain can be felt at the top of the arm just above the elbow and is worse on reaching around to the back, difficulty sleeping and reaching up. Common investigations for this condition are simple plain x-ray, ultrasound or MRI scan of the shoulder.
Treatment can include physiotherapy including acupuncture and massage, steroid injections carried out in an out-patient setting or arthroscopic / keyhole surgery. Arthroscopic surgery is generally safe and reliable and has around an 85 to 90% success rate. Arthroscopic surgery is performed through three holes into the shoulder, one at the front, one at the side and one at the back. The surgery involves removing any inflamed tissue, debridement of the tendons and shaving off some of the acromion bone (hooked bone) and its leading edge in order to open up the space for the tendons to move around more easily. If your imaging and assessment shows pain coming from the AC joint which could be arthritic, then a few millimetres of your end of your collar bone (clavicle) may be removed as well. Surgery is usually carried out as a day case so you are able to go home the same day. It is commonly done under a general anaesthetic with a regional block (injection into the nerves in the neck which will anaesthetise the arm so when you wake from surgery although the arm will feel numb and weak it should feel very comfortable).
The risks involved with arthroscopic surgery are infection, bleeding, nerve injury, pain and stiffness. Average recovery is anywhere between six weeks up to three to four months.
With AC joint excision recovery can be longer and it can take up to six months for symptoms to completely settle down.
If at the time of surgery your tendons require repair, then recovery is much more prolonged. Pre-operatively I will assess the size of the tear and the state of the tissues depending on your imaging. Repair is again carried out arthroscopically which may mean an extra hole on the side of the shoulder. Repair is generally carried out with bone anchors (similar to a small wall plug). Some anchors are all now suture material. Sutures are passed with arthroscopic instruments through the tendons and secured down with knots in order to reattach the tendon to the bone. Surgery takes about one to two hours but this does depend on the size of the tear and, as already stated, recovery can be more protracted. With repair the shoulder may need to be protected for up to four to six weeks in a sling with a large tear and physiotherapy will be required for three months post operatively. The same surgical risks apply as for the decompression but there will be to a certain extent a larger degree of stiffness and slightly longer recovery. Surgery can still be performed as a day case. There is a risk of re-rupture although patients can benefit from significant pain relief even with re-rupture following arthroscopic surgery.
Symptomatology: The Arthritic Shoulder
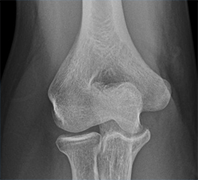
Arthritis of the ball and socket (glenohumeral joint) occurs with age. It is most common after a previous injury but can develop spontaneously with no history of trauma. Patients are often a little older towards the age of 60 to 70 and again there is often a dull ache generally within the shoulder, aching in bed at night, loss of movement with pain and crepitus (grinding sensation within the shoulder on movement). Classically loss of external rotation is very common (turning the arm out to the side) and this particular movement is very restricted.
If your shoulder is arthritic, it is essential to have imaging in the form of plain x-ray and possibly MRI or CT scan to assess the bone in more detail.
Treatment can include analgesics and anti-inflammatories, physiotherapy, injection treatment or surgery in the form of shoulder replacement.
Total Shoulder Replacement / Arthroplasty:
There are three main forms of shoulder replacement that are available for treatment for an arthritic shoulder. Treatment will depend on the quality of the bone and the quality of the tendons around the shoulder (whether the rotator cuff tendons are intact and functional). Patient’s age and functional demands must be considered and co-morbidities.
Treatment can include the following:
- Hemi-arthroplasty and resurfacing, replacing the ball part of the joint only.
- Replacement of the ball and socket with anatomical total shoulder replacement
- Reverse polarity shoulder replacement (reverse meaning that the ball part is attached to the socket and a cup is attached to the humerus (arm bone).
Any of the above surgery will require a general anaesthetic, an incision on the front or side of the shoulder. Surgery can take anywhere between one to two hours. With surgery there are risks of infection, bleeding, nerve injury and fracture.
Unlike knee and hip replacements, the stay in hospital is a lot shorter with shoulder replacement but this will depend on whether you have any other medical problems. Most patients go home within one to two days of their surgery. You will need to maintain a sling for four weeks post operatively and you will require three to four months of physiotherapy.
Improvement in pain and function can extend up to anywhere between six and twelve months following the surgery. General recovery is anywhere between four and six months on average.
A reverse shoulder replacement is reserved for patients whose tendons have either torn or are non-functional around the shoulder.
Symptomatology: Shoulder dislocation / Instability
Shoulder dislocations are divided into two categories. You will have either dislocated your shoulder from an injury or from very minimal movement and your shoulder has popped out and gone back into joint fairly rapidly.
Where a dislocation has occurred without an injury, this may indicate that you have a pre-requisite to instability of the shoulder, possibly even in the opposite shoulder and other joints. This may be a sign of generalised joint laxity (hypermobile joints).
For a shoulder dislocation that occurs without injury, surgery is not recommended for this and the best treatment is physiotherapy.
If your shoulder dislocation occurs from an injury and if you go on to have further symptoms then you may require further investigations and potentially surgical treatment. It is a very common injury in contact sports, particularly in rugby and overhead sports such as basketball. Persisting symptoms such as apprehension, symptoms of instability and further dislocation to occur are much more common in patients of a younger age group.
With a traumatic dislocation of the shoulder, it is essential to assess your shoulder and examine for any other signs of any other tendon damage. You will require x-ray, most likely an MR arthrogram (MRI scan with dye injected into the shoulder in order to highlight some of the structures around the socket of the joint) or possibly a CT scan.
Surgery for dislocation involves arthroscopic stabilisation. This is keyhole surgery and involves a hole at the back of the shoulder and two at the front. When the shoulder is forced out the front it tears the lining of the socket. This can be repaired through keyhole surgery using small anchors which are drilled into the edge of the socket, these have sutures (strings within the anchor) which are then passed through the edge of the socket and secured down in order to stabilise the joint. Surgery takes about one hour. The patient can go home the same day and the arm is rested in a sling for two weeks. Recovery can take from three to four months. Average return to sport, particularly contact sports is about three to four months. The risk of re-dislocation is still higher than the average population and the younger you are the higher this is. Current studies show that there is a 6% re-dislocation rate with arthroscopic techniques at two to five years.
The other risks with this surgery include infection, pain, stiffness, bleeding and nerve injury. There is a small risk of some permanent stiffness. This may manifest itself by slightly reduced external rotation (turning the arm out to the side) and elevating the arm up above the head with the elbow flexed. Physiotherapy can improve this but it is not uncommon to have some degree of permanent stiffness.
If your investigations show that there is bone loss on the socket or at the back of the humeral head (ball joint) then more extensive open surgery may be indicated. If the shoulder has dislocated on a number of occasions, as the ball part slides over the front of the socket this may scuff the edge of the socket and obviously the surface area is reduced. If this is the case then open surgery may be required in the form of bone grafting (a modified Laterjet procedure). This involves an incision on the front of the shoulder and bone is taken from the edge of the scapula or from the edge of your pelvis and fixed with two screws onto the front edge of the socket, the surrounding soft tissues of the capsule are then secured and tightened as well. The rehabilitation and recovery is essentially the same as for arthroscopic surgery but with open surgery there are risks of the bone graft and metalwork in the shoulder.
Symptomatology: Shoulder injuries – Falling on the shoulder
After a fall onto the shoulder, whether it is off a bicycle or injury playing sport, there are a large number of injuries that need to be considered. These can include the following:
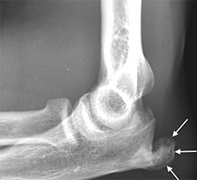
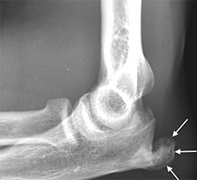
Clavicle (collarbone) fracture – with the increasing popularity of cycling, clavicle fracture is very a common condition and is caused by a fall on the outside of the shoulder. There is immediate pain and crepitus, swelling and bruising around the clavicle. X-rays will be required and the general consensus today is if there is a lot of comminution (multiple fragments around the fracture site) or there is significant overlap of the broken ends of the bone, then the outcome is better with surgical fixation. Surgery is done under general anaesthetic and an incision is made over the clavicle, the fracture ends are held together back in an anatomical position and a plate placed on the clavicle. This is secured with screws. An overnight stay in hospital is required and you will need to wear a sling for up to six weeks and further x-rays will be needed. Union of the fracture (healing) can take up to three to five months for complete union on x-ray. There are risks of infection, bleeding and it is quite common to have some degree of numbness around the edge of the scar, problems with metalwork and non-union (non-healing) of the fracture can occur in 6 and 8% of cases. In very slim patients and the younger population removal of the metalwork may need to be considered.
AC joint injury – A fall onto the outside of the shoulder or even outstretched hand can cause an AC joint injury. Patients normally have instant pain over the top of the shoulder and a large lump over the AC joint. The AC joint is where the collarbone (clavicle) meets the scapula. There are ligaments holding the clavicle down in line and these will have ruptured. A small degree of displacement may not require any intervention but it can still take up to three months for the pain to settle and function to return to normal. It is often advised to remain in a sling for six weeks.
If the displacement is significant, or there is a prominent lump and the patient is getting significant pain and functional restrictions, one may consider reconstructing the AC joint. This again requires open surgery under a general anaesthetic. Approximately a three inch bra strap (in line with the typical bra strap) incision is made over the top of the clavicle and the clavicle is pushed down into its normal position. My preference currently is to use an artificial ligament which raps around the coracoid (a bony beak of bone which projects from the scapula) and the ligament is passed up through the clavicle and secured with two screws to maintain stability of your clavicle and alignment. Soft tissues are then repaired over the top of the shoulder. This is again carried out as an overnight stay and you will need to remain in a sling for six weeks and will need physiotherapy. Recovery is usually around three months.







